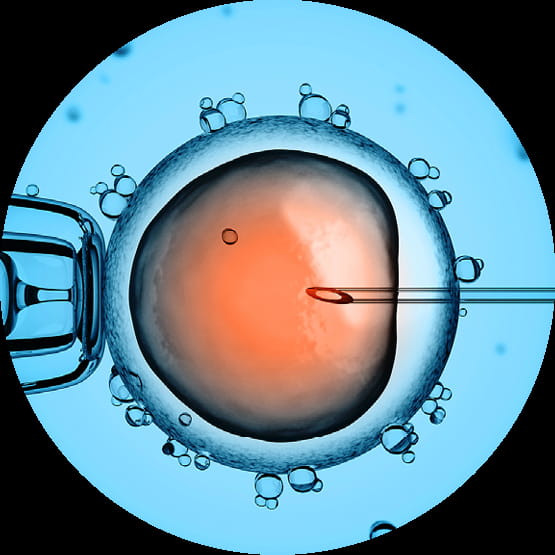
In principle, ICSI is similar to in vitro fertilisation as here the
egg is also fertilised in a Petri dish. The main difference is that
in the case of ICSI, a spermatozoon is injected directly into the egg.
How does ICSI work?
Under a microscope, the egg is captured using a pipette and the sperm injected through the zona pellucida directly into the egg using a hypodermic needle.
This procedure increases the chances of fertilisation significantly even if the results of semen tests are poor. Subsequently, fertilised eggs are allowed to develop in a special incubator and after 2 to 5 days they are transferred to the uterus of the woman.
We use a time-lapse camera to record images of embryos at regular intervals, enabling us to identify that embryo that is best developing and has the best chances of successful implantation.
ICSI is particularly indicated if the result of the sperm test of the male partner is poor. If too few healthy spermatozoa are available, if they display reduced motility or feature an increased deformity rate, an intracytoplasmic sperm injection may be the optimum treatment option.
In the case of blocked vas deferens or of a congenital bilateral absence of the vas deferens, or if there are no spermatozoa present in the ejaculate, the semen can be retrieved from the testicles or epididymis by means of a minor surgical procedure - either TESE (testicular sperm extraction) or TESA (testicular sperm aspiration).
The subsequent preparation in the embryology laboratory serves to sort out spermatozoa of a poor quality. The healthy spermatozoa undergo the crucial maturation process and are therefore capable of fertilisation. This procedure ensures that the child has the same genetic heredity as the man.
Spermatozoa which are no longer required for the moment are frozen in our institute and can thus be resorted to for another fertilisation process at a later time.
Depending on the age of the partners, the results of examinations and other influencing factors, such as stress, consumption of alcohol and tobacco and obesity, there is a 40% chance of achieving a pregnancy per cycle.
The physiological process is simulated in a Petri dish with the help of hyaluronic acid. Only those spermatozoa that bind to the acid - i.e. that have developed the corresponding receptors and are thus mature - are selected and used for fertilisation by means of PICSI.
Medical studies have demonstrated that spermatozoa with receptors and at the appropriate level of maturity have greater DNA integrity. PICSI is only really indicated if the result of semen testing is poor, but a sufficient number of mobile spermatozoa is also required. As a result, there have been repeated reports of failed fertilisation and even miscarriages in association with the corresponding patient group.
Hyaluronic acid is not only used for PICSI but can also be used to assess the quality of semen samples in a binding test for the purposes of evaluation. A PICSI Petri dish test will show the number of mature spermatozoa with receptors in the ejaculate; on this basis, we can provide further advice on appropriate treatment.
In the video recording can be seen both free-swimming spermatozoa in the general area and others close to the hyaluronic acid (circular area); these are bound by their receptors on the head to the hyaluronic acid on the base of the dish. Their tails are still rotating. The numbers of these spermatozoa are counted during the binding test and can be selected for use in PICSI.
A Petri dish and hyaluronic acid are used. Hyaluronic acid is naturally present around the eggs in the uterus. As a physiological substance, it thus has no negative side effects on spermatozoa or eggs. Only mature spermatozoa have the necessary receptors that enable them to bind to hyaluronic acid. In this way, nature ensures that only mature spermatozoa are capable to reaching the eggs.